Urinary Incontinence
What Is Urinary incontinence?
Urinary incontinence is the accidental or unwanted leakage of urine. There are many Iranian have some type of bladder control problem, and most are women. Although about half of the elderly have episodes of incontinence, bladder problems are not a natural consequence of aging, and they are not exclusively a problem of the elderly. Urinary incontinence can develop at any age, but as we get older it becomes more common because of changes in the body and illness that effect bladder function. However, studies show that only about 30 percent of people with incontinence seek treatment. Embarrassment or the belief that there is nothing that can be done may stop women from seeking treatment.
What are causes of urinary incontinence?
Most healthy people will empty their bladder about every three to four hours (four to eight times in 24 hours). Getting up once at night to urinate is normal. But getting up more often at night, leaking urine when doing activities, or not being able to hold your urine until you reach a nearby bathroom is not normal.
Older men can become incontinent as the result of prostate surgery. Pelvic trauma, spinal cord damage, caffeine, or medications, including cold preparations and diet drugs that are available over-the-counter, can also cause episodes of Urinary incontinence. Diseases which affect the nerves that control the bladder, such as multiple sclerosis, can be associated with urinary incontinence.
Other factors that contribute to bladder incontinence include decreased mobility or impaired thinking (such as forgetfulness, confusion, or senility), particularly in combination with drugs such as sedatives, sleeping pills, and alcohol.
What are the types of urinary incontinence?
There are four common types of incontinence:
- Stress incontinence happens when the bladder can't handle the increased compression during exercise, coughing, or sneezing. This form of incontinence usually occurs in women under 60 and in men who have had prostate surgery.
- Urge incontinence is caused by a sudden, involuntary bladder contraction. This form is more common in older adults.
- Mixed incontinence is a combination of both stress and urge incontinence, and is most common in older women.
- Overflow incontinence, in which the bladder becomes too full because it can't be fully emptied, is a rarer type of the disorder. The condition is caused by a bladder obstruction or injury. In men, it can be the result of an enlarged prostate.
How is urinary incontinence diagnosed?
Medical History
The first step in solving a urinary problem is talking to your health care provider. Your general medical history, including any major illnesses or surgeries, and details about your continence problem and when it started will help your doctor determine the cause. You should also talk about the medicines you take, both prescription and nonprescription, because they might be part of the problem.
Voiding Diary
You may be asked to keep a voiding diary, which is a record of fluid intake and trips to the bathroom, plus any episodes of leakage. Studying the diary will give your health care provider a better idea of your problem and help direct additional tests.
Physical Examination
A physical exam will check for prostate enlargement or nerve damage. This exam gives the doctor a general idea of the size and condition of the prostate gland. To check for nerve damage, the doctor may ask about tingling sensations or feelings of numbness and may check for changes in sensation, muscle tone, and reflexes.
Urodynamics
Urodynamic testing focuses on the bladder's ability to store urine and empty steadily and completely, and on your sphincter control mechanism. It can also show whether the bladder is having abnormal contractions that cause leakage. The testing involves measuring pressure in the bladder as it is filled with fluid through a small catheter. This test can help identify limited bladder capacity, bladder overactivity or underactivity, weak sphincter muscles, or urinary obstruction.

How is urinary incontinence treated?
No single treatment works for everyone. Your treatment will depend on the type and severity of your problem, your lifestyle, and your preferences, starting with the simpler treatment options. Many patients regain urinary control by changing a few habits and doing exercises to strengthen the muscles that hold urine in the bladder. If these behavioral treatments do not work, you may choose to try medicines or a continence device-either an artificial sphincter or a catheter. Finally, for some men, surgery is the best choice.
Here are commonly recommended treatments:
- Pelvic Muscle Rehabilitation-to improve pelvic muscle tone and prevent leakage.
- Kegel exercises. Regular, daily exercising of pelvic muscles can improve, and even prevent, urinary incontinence. This is particularly helpful for younger women. Should be performed 30-80 times daily for at least 8 weeks.
- Biofeedback. Used in conjunction with Kegel exercises, biofeedback helps people gain awareness and control of their pelvic muscles.
- Vaginal weight training. Small weights are held within the vagina by tightening the vaginal muscles. Should be performed for 15 minutes, twice daily, for 4 to 6 weeks.
- Pelvic floor electrical stimulation. Mild electrical pulses stimulate muscle contractions. Should be done in conjunction with Kegel exercises.
- Behavioral Therapies-to help people regain control of their bladder.
- Bladder training teaches people to resist the urge to void and gradually expand the intervals between voiding.
- Toileting assistance uses routine or scheduled toileting, habit training schedules, and prompted voiding to empty the bladder regularly to prevent leaking.
Medications
Anticholinergics (Oxybutynin Tolterodin) prevent urge incontinence by relaxing Detrusor muscles and are indicated for the treatment of an overactive bladder with symptoms of urinary frequency, urgency, or urge incontinence.
Estrogen, either oral or vaginal, may be helpful in conjunction with other treatments for postmenopausal women with urinary incontinence.
Alpha-blockers: Terazosin (Hytrin), doxazosin (Cardura), tamsulosin (Flomax), and alfzosin (Uroxatral) are used to treat problems caused by prostate enlargement and bladder outlet obstruction. They act by relaxing the smooth muscle of the prostate and bladder neck, allowing normal urine flow and preventing abnormal bladder contractions that can lead to urge incontinence
Catheters
- Clean intermittent catheterization: If you have problems emptying your bladder because of an enlarged prostate or because of nerve damage, you may use a catheter at regular times, or as needed, to drain urine and prevent overflow incontinence. Depending on your situation, the catheterization may be done for you, or you may learn to do it yourself. You will need to learn sterile technique to avoid urinary tract infections.
- Condom catheter: Some men may prefer a drainage system that fits over the penis like a condom. You must take the same care to avoid infection as you do with other catheters. Condom catheters can also carry a risk of skin breakdown.
Botox injection
Botox therapy has been used for the treatment of refractory urge incontinence. Most of the studies so far have been on patients with neurologic problems and it is not yet FDA approved for use in the bladder although there will soon be clinical trials.
Urethral Injections
Another method to help keep the urethra closed is to inject a fat-like substance into the area that surrounds the opening of the bladder into the urethra. A variety of bulking agents are available for injection. Your doctor will discuss which one may be best for you. Urocol, for example, is a synthetic material. After using local anesthesia or sedation, a doctor can inject the material in posterior urethra. Over time, the body slowly eliminates the material, so you may need repeat injections.


A- Cystoscopic view of bladder neck in incontinent patient B- The same patient after UROCOL injection
Artificial Sphincter
Some men may eliminate urine leakage with an artificial sphincter, an implanted device that keeps the urethra closed until you are ready to urinate. This device can help people who have incontinence because of weak sphincter muscles or because of nerve damage that interferes with sphincter muscle function. It does not solve incontinence caused by uncontrolled bladder contractions.
Surgery to place the artificial sphincter requires general or spinal anesthesia. The device has three parts: a cuff that fits around the urethra, a small balloon reservoir placed in the abdomen, and a pump placed in the scrotum. The cuff is filled with liquid that makes it fit tightly around the urethra to prevent urine from leaking. When it is time to urinate, you squeeze the pump with your fingers to deflate the cuff so that the liquid moves to the balloon reservoir and urine can flow through the urethra. When your bladder is empty, the cuff automatically refills in the next 2 to 5 minutes to keep the urethra tightly closed.
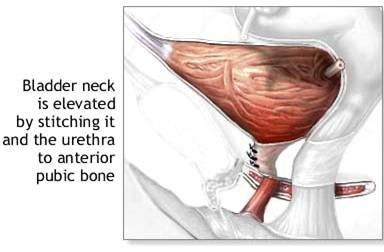
BLADDER NECK SUSPENSION PROCEDURES
There are an enormous number of bladder neck suspension procedures, most of which are minor variations on a theme. In every case, the bladder neck suspension procedure involves placing stitches between the ligaments and tendons that support the bladder neck and urethra and tying these stitches to a strong supporting structure, usually the pubic bone or an attachment of dense fascia or a ligament right at the pubic bone. In this way, the bladder neck and urethra are stabilized against coughing, straining, and exercising so that the urethra will not open and leak. Almost all the bladder neck suspension procedures are effective treatments for stress urinary incontinence caused by urethral hypermobility (poor support). The bladder neck suspension procedures are further divided into those that are performed primarily through the vagina and those that are performed primarily through an abdominal incision.
Sling
In a sling procedure, the surgeon creates a support for the urethra by wrapping a strip of material around the urethra and attaching the ends of the strip to the pelvic bone. The sling keeps constant pressure on the urethra so that it does not open until the patient consciously releases the urine.
The basic concept of the sling is that a piece of strong connective tissue (fascia) is harvested from one portion of the body (usually from the covering of the rectus muscle of the abdomen) and is then placed underneath the urethra and bladder neck as a supporting "hammock". The sling thus corrects the poor anatomic support of the bladder neck and additionally provides a degree of compression and coaptation to the proximal urethra, correcting intrinsic deficiency of the urethra. Slings can be composed of fascia from the abdomen (rectus), the leg, fascia lata, cadaver fascia, and synthetic material. In addition, a sling procedure has been described in which the native fascia at the bladder neck and urethra is reconstructed/re-supported, to create a local sling that extends to support and coapt the proximal urethra (the vaginal wall sling procedure).
Urinary Diversion
If the bladder must be removed or all bladder function is lost because of nerve damage, you may consider surgery to create a urinary diversion. In this procedure, the surgeon creates a reservoir by removing a piece of the small intestine and directing the ureters to the reservoir. The surgeon also creates a stoma, an opening on the lower abdomen where the urine can be drained through a catheter or into a bag.
Urinary Incontinence at a Glance
- Urinary incontinence (UI) is not exclusively a problem of the elderly.
- UI is not a natural consequence of aging.
- UI has a number of causes.
- There are several types of UI.
- Treatment for UI depends on the type of incontinence, its causes, and the capabilities of the patient.
Impotence
Erectile dysfunction (ED) is the inability of a man to achieve or maintain an erection sufficient for his sexual needs or the needs of his partner. Most men experience this at some point in their lives, usually by age 40, and are not psychologically affected by it.
Frequent erectile dysfunction can cause emotional and relationship problems, and often leads to diminished self-esteem. Erectile dysfunction has many causes, most of which are treatable, and is not an inevitable consequence of aging.
Sexual dysfunction is an extremely common problem affecting over 50% of men between the ages of 40 and 70. With newer treatments available, public awareness of the problem has increased greatly. Commonly, however, one may experience partial erection with either incomplete rigidity or loss of rigidity before ejaculation. In the past physicians often attributed ED to psychological causes. However, we now know that psychogenic impotence is responsible for less than 10% of cases of serious erectile dysfunction. Common causes of ED include medications for other conditions, arterial blockage due to atherosclerosis, peripheral nerve damage due to diabetes, pelvic fracture, and spinal cord injury. Fortunately, determining the specific cause of erectile dysfunction is usually not necessary as treatment is fairly standard.
Physiology of Erection
The physiological process of erection begins in the brain and involves the nervous and vascular systems. Neurotransmitters in the brain (e.g., epinephrine, acetylcholine, nitric oxide) are some of the chemicals that initiate it. Physical or psychological stimulation (arousal) causes nerves to send messages to the vascular system, which results in significant blood flow to the penis. Two arteries in the penis supply blood to erectile tissue and the corpora cavernosa, which become engorged and expand as a result of increased blood flow and pressure.
Because blood must stay in the penis to maintain rigidity, erectile tissue is enclosed by fibrous elastic sheathes (tunicae) that cinch to prevent blood from leaving the penis during erection. When stimulation ends, or following ejaculation, pressure in the penis decreases, blood is released, and the penis resumes its normal shape.
What causes erectile dysfunction?
The following medical problems can cause erectile dysfunction:
- Diabetes (high blood sugar)
- Hypertension (high blood pressure)
- Atherosclerosis (hardening of the arteries)
- If you can't keep your blood sugar or your blood pressure under control, you can get erectile dysfunction. It's important that you take your medicines for these problems just the way your doctor tells you.
- Sometimes your hormones get out of balance and this causes erectile dysfunction. Your doctor will decide if you need blood tests to check your hormones.
- Some medicines can cause erectile dysfunction. If this is true for you, your doctor may take you off that medicine or give you a different one. Drinking too much alcohol, smoking too much and abusing drugs can also cause erectile dysfunction.
- Problems in your relationship with your sexual partner can also cause erectile dysfunction. Improving your relationship may help your sex life. If you decide to seek therapy, it will probably be most effective if your sex partner is included. Couples can learn new ways to please one another and to show affection. This can reduce anxiety about having erections.
Physical causes of erectile dysfunction:
Alcohol and tobacco use, fatigue, brain or spinal-cord injuries ,hypogonadism (which leads to lower testosterone levels) , liver or kidney failure, multiple sclerosis parkinson's disease, radiation therapy to the testicles, stroke, some types of prostate or bladder surgery
Diagnosis of Impotence (Erectile Dysfunction)
The diagnosis of erectile dysfunction is established through a detailed visit with your doctor that is designed to evaluate for all of the causes listed above. This can usually be accomplished through a series of questions and a detailed physical examination. Further tests may be necessary to look for some of the physical or medical causes of ED. Blood tests to measure blood sugar, kidney and liver function and hormone levels may be ordered. More specialized tests include an ultrasound of the genital area to view it?s blood vessel anatomy and measure the blood flow characteristics of the area. This may involve scanning before and after an injection of a drug that creates an erection. Less commonly, more invasive tests may be used if vascular problems are suspected. Cavernosometry is a test that measures the pressure in the penile blood vessels and the sponge-like penile tissue. It assesses if blood flow to the area is adequate for forming an erection. Cavernosography involves the injection of radiographic dye into the penile blood system to see if there is an abnormal leakage of blood out of the sponge-like tissue that is preventing the proper accumulation of blood necessary to create an erection.
Laboratory Tests
Several laboratory tests can help diagnose impotence. Tests for systemic diseases include blood counts, urinalysis, lipid profile, and measurements of creatinine and liver enzymes. For cases of low sexual desire, measurement of testosterone in the blood can yield information about problems with the endocrine system.
Other Tests
Duplex ultrasound– Duplex ultrasound is used to evaluate blood flow, venous leak, signs of artherosclerosis, and scarring or calcification of erectile tissue. Erection is induced by injecting prostaglandin, a hormone-like stimulator produced in the body. Ultrasound is then used to see vascular dilation and measure penile blood pressure (which may also be measured with a special cuff). Measurements are compared to those taken when the penis is flaccid.
Penile nerve function– Tests such as the bulbocavernosus reflex test are used to determine if there is sufficient nerve sensation in the penis. The physician squeezes the glans (head) of the penis, which immediately causes the anus to contract if nerve function is normal. A physician measures the latency between squeeze and contraction by observing the anal sphincter or by feeling it with a gloved finger inserted past the anus. Specific nerve tests are used in patients with suspected nerve damage as a result of diabetes or nerve disease.
Nocturnal penile tumescence (NPT)– It is normal for a man to have five to six erections during sleep, especially during rapid eye movement (REM). These erections occur about every 90 minutes and last for about 30 minutes. Their absence may indicate a problem with nerve function or blood supply in the penis. There are two methods for measuring changes in penile rigidity and circumference during nocturnal erection: snap gauge and strain gauge.
Penile biothesiometry–This test uses electromagnetic vibration to evaluate sensitivity and nerve function in the glands and shaft of the penis. A decreased perception of vibration may indicate nerve damage in the pelvic area, which can lead to impotence.
Vasoactive injection– When injected into the penis, certain solutions cause erection by dilating blood vessels in erectile tissue. Normally, these injections produce an erection lasting about 20 minutes. During this procedure, penile pressure is measured and x-rays may be taken of the penile blood vessels using a special dye (contrast agent).
Treatment
Various Options
Most physicians suggest that treatments for impotence proceed along a path moving from least invasive to most invasive. This means cutting back on any harmful drugs is considered first. Psychotherapy and behavior modifications are considered next, followed by vacuum devices, oral drugs, locally injected drugs, and surgically implanted devices (and, in rare cases, surgery involving veins or arteries).
Lifestyle changes & prevention
- A healthier lifestyle can often be beneficial and can help prevent any further deterioration caused by underlying medical conditions.
- If you smoke, make a plan to stop.
- Take moderate-intensity exercise (so you feel warm and slightly out of breath - brisk walking for instance - for half an hour on most days of the week.
- Eat a balanced diet rich in fruit and vegetables and low in fat.
- Drink alcohol in moderation. Other recreational drugs can cause ED.
- Aim to reduce stresses in your life by looking at the balance between your work and your home/leisure time.
- Relaxation techniques may be helpful.
Psychotherapy
Experts often treat psychologically based impotence using techniques that decrease anxiety associated with intercourse. The patient's partner can help apply the techniques, which include gradual development of intimacy and stimulation. Such techniques also can help relieve anxiety when physical impotence is being treated.
Erection-inducing drugs
Oral drugs which induce erection have revolutionised the treatment of ED over the last eight years. They don’t work for everybody, but they do work for the majority – even in diabetes. They can also help people with neurological and spinal problems.
Also, the choice of available drugs means that if one particular drug doesn’t suit you, it’s well worth trying one of the others.
They all have side-effects, only a few of which we can list here. For more information, read the package insert leaflet, and if in doubt ask your doctor.
It is not safe for some people to use these drugs, and some medications interact dangerously with them. Therefore, before going on any of these pills you should always see a doctor, talk things over with him, and have a physical check-up.
The oral drugs currently available are:
- Viagra tablets (sildenafil)
- Cialis tablets (tadalafil)
- Levitra tablets (vardenafil)
Widens the bloods vessels, so giving an erection - provided the penis is rubbed. In most men, works within an hour. Effect lasts for about four hours. Easily blocked by food in the stomach.
Viagra still remains the world’s most popular ED drug. The most common side-effects are headache, visual disturbances, blocked nose, flushed face, indigestion, palpitations - and dizziness after getting out of bed too quickly! .Viagra is very dangerous with certain heart drugs. Interacts with many medications. Do not drink grapefruit juice on day of use.
Self-Injection. One or more drugs (papaverine, phentolamine and prostaglandin-E1) can be injected into the penis to increase blood flow. The injection is nearly painless and produces a more natural erection than a vacuum device or implant. However, until the proper dose is worked out, a man might have a prolonged and painful erection. In rare instances, an erection that does not go down after ejaculation may require surgery.
Vacuum Devices
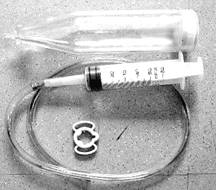
Mechanical vacuum devices cause erection by creating a partial vacuum around the penis, which draws blood into the penis, engorging it and expanding it. The devices have three components: a plastic cylinder, in which the penis is placed; a pump, which draws air out of the cylinder; and an elastic band, which is placed around the base of the penis, to maintain the erection after the cylinder is removed and during intercourse by preventing blood from flowing back into the body.
What about surgery?
The types of surgery which are available for ED are as follows.
Curing a venous leak- A few men lose their erections because blood leaks out of the penis through a leakage in the veins. Occasionally, this leak only occurs in certain sex positions. Where a leak can be clearly pin-pointed by special X-rays, a urologist may be able to operate in order to improve matters.
Insertion of internal splints- A skilled urologist can insert artificial splints inside the body of the penis. With the simplest type of splint (which is just a firm rod), the man lifts the organ into a vertical position when he wants to have intercourse. There are more sophisticated (and much more expensive) internal splints which you or your partner can inflate when you wish to make love. Some couples report being very pleased with these. But if anything goes wrong with the surgery – for instance, infection or bleeding, you could be in some. The two major types are:
Malleable Rods. Two long rods (also referred to as semi-rigid prostheses) are inserted into the outer channels of the penis through a small incision in the lower abdomen or scrotum. However, they can be bent close to the body for concealment. Because there are no moveable or inflatable parts, malfunctions are rare.

Inflatable Cylinders. These devices consist of one or two inflatable cylinders, a finger-activated pump and an internal reservoir that stores liquid used to inflate the tubes. All components--the cylinders, pump and reservoir--are implanted within the penis, scrotum and lower abdomen respectively. When the pump in the scrotum is manually squeezed several times, the fluid from the reservoir is released into the cylinders. They expand and create an erection, which is maintained until the release valve on the pump is squeezed to return the fluid to the reservoir.

Points to Remember
Erectile dysfunction (ED) is the repeated inability to get or keep an erection firm enough for sexual intercourse.
-
ED affects 15 to 30 million American men.
-
ED usually has a physical cause.
-
ED is treatable at all ages.
-
Treatments include psychotherapy, drug therapy, vacuum devices, and surgery.